Tuberculosis (TB) Test: What It Is, How It Works, Results & Side Effects
October 10,2025
A cough that won’t quit? Close contact with someone who has TB? Or you just need clearance for work. Whatever brought you here, let’s make tuberculosis testing simple. We’ll cover the TB test options (skin vs. blood), when each makes sense, what results really mean, and which diagnostic tests for TB confirm active disease, so you can act confidently.
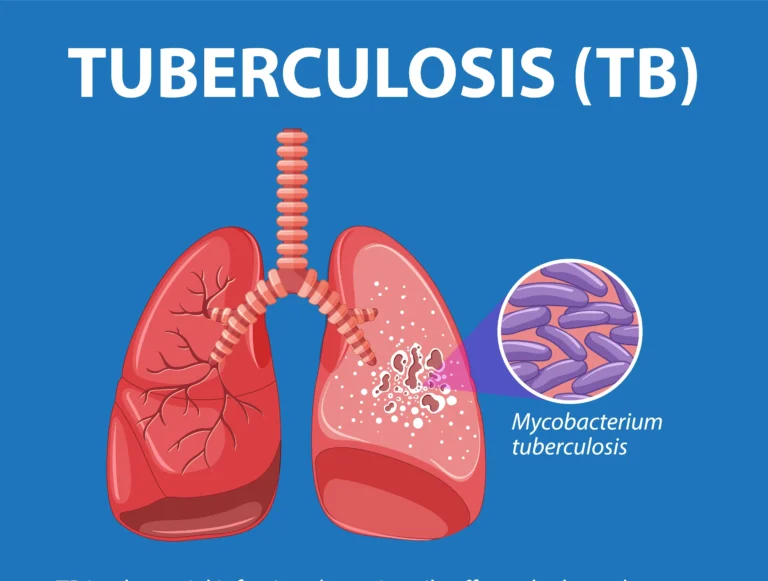
What Is a TB Test (and What It’s Not)?
A tuberculosis test, either the TB Mantoux test (skin) or a TB blood test (IGRA), checks whether your immune system has ever seen TB bacteria. It doesn’t tell you if infection is currently active or latent; you’ll need confirmatory testing for that (e.g., sputum tests, NAAT like Xpert, and chest imaging).
Quick definitions
TB blood tests (IGRAs): Lab tests (e.g., QuantiFERON-TB, T-SPOT) that measure immune response to TB-specific antigens. No return visit for reading. Often preferred if you’ve had the BCG vaccination.
TB Mantoux test / TST: A tiny amount of tuberculin (PPD) is injected under the skin and the raised bump (induration) is measured 48–72 hours later.
Who Should Get a Tuberculosis Test?
You’ll likely need a TB test if you:
- had close contact with a person with active TB;
- work in healthcare or live/work in congregate settings (hostels, shelters, prisons, long-term care);
- are immunocompromised (HIV, chemo, transplant meds, high-dose steroids);
- were born in/traveled to regions where TB is common; or
- have symptoms suggesting active TB (persistent cough, fever, night sweats, weight loss).
How often? High-risk groups may need annual screening; low-risk adults generally test only after exposure or when required for work/school. Follow your provider’s advice and local policy.
Choosing the Right Test: Mantoux vs. Blood (IGRA)
TB Mantoux Test (TST) — the classic “bump test”
- Good for: Children <5 years and general screening where follow-up is easy.
- Limits: BCG can cause false-positive skin tests; it requires a return visit to read.
TB Blood Test (IGRA) — the one-and-done lab draw
- Good for: People who received BCG, those unlikely to return for a reading, and many healthcare workers.
- Advantages: One visit; fewer false positives from BCG.
Not sure which to pick? If you’ve had BCG or can’t come back in 48–72 hours, an IGRA is often preferred.
What to Expect: The TB Testing Process
TB Mantoux Test (TST)
- Tiny PPD injection under your forearm; a small wheal forms.
- Return in 48–72 hours so a trained clinician can measure the induration (the firm bump), not the redness.
How big is “positive”? Depends on your risk:
- ≥5 mm: Positive for people with HIV, recent close contacts, abnormal chest X-ray, or marked immunosuppression.
- ≥10 mm: Positive for healthcare workers, recent arrivals from high-TB regions, people with certain medical conditions.
- ≥15 mm: Positive for people with no known risk factors.
TB Blood Test (IGRA)
One blood draw → lab mixes your blood with TB antigens → reports positive/negative/indeterminate (usually within 1–2 days).
Side effects? Minimal brief needle sting, occasional light bruising.
“Positive” Doesn’t Mean “Contagious”: What Results Really Mean
- Positive TST/IGRA = your immune system recognizes TB. You may have latent TB infection (LTBI) or active TB; screening alone can’t distinguish.
- Negative TST/IGRA = TB is less likely, but still possible if you’re immunosuppressed or tested too soon after exposure; repeat testing ~8–10 weeks after exposure may be advised.
That’s why screening is step one. Next comes the lab diagnosis of TB to rule in/out active disease.
Lab Diagnosis of TB: Confirming Active Infection
If screening is positive or you have symptoms, clinicians move to diagnostic tests for tuberculosis:
1) Sputum tests (for pulmonary TB)
- Smear microscopy: Rapid but less sensitive.
- Culture: Gold standard; identifies TB and drug susceptibility (weeks).
- NAAT / Xpert MTB/RIF or Ultra: Rapid molecular test detecting TB DNA and rifampicin resistance in <2 hours.
2) Imaging
- Chest X-ray/CT support diagnosis but are not definitive without microbiology.
3) Extrapulmonary TB
- Samples from the affected site (e.g., lymph node, CSF, pleural fluid, urine) for smear/culture/NAAT. WHO recommends Xpert (including Ultra) as an initial test in many adult and pediatric scenarios.
Treatment & Why Completing It Matters
- Latent TB infection (LTBI): Short rifamycin-based regimens (e.g., 3HP once-weekly isoniazid + rifapentine for 12 weeks, or 4R rifampin for 4 months) are preferred and reduce progression to active TB.
- Active TB disease: Multi-drug therapy for months; exact regimen depends on drug susceptibility. Adherence is critical; incomplete treatment fuels drug-resistant TB, so programs like DOT (Directly Observed Therapy) may be used.
Preventing Transmission
- Test promptly if exposed or symptomatic.
- Follow isolation guidance when active TB is suspected/confirmed.
- Ensure household/close contacts are screened.
- Improve ventilation and use masks in high-risk settings.
Conclusion: Test Smart, Act Fast, Finish Strong
If you’ve got risk factors or symptoms, a TB test (skin or blood) is a smart first step. If it’s positive, or you’re unwell, move quickly to diagnostic tests for TB (sputum NAAT, culture, imaging) so you get answers, not guesses. And if treatment is prescribed, finish every dose. That’s how you protect yourself, your family, and your community.
CTA: Think you were exposed, starting a new job, or dealing with a stubborn cough? Book a tuberculosis test today, and ask whether a TB Mantoux test or an IGRA blood test is right for you.
FAQs: TB Test & Diagnosis
1) Is the TB skin test or the TB blood test more accurate?
Both are strong screens. IGRAs are more specific if you’ve had BCG and don’t require a return visit; TST is widely available and reliable when follow-up is easy.
2) Can a TB test tell if I’m contagious?
No. TST/IGRA only shows immune memory. Active TB (and contagiousness) is confirmed with lab diagnosis of TB sputum tests, NAAT, culture, and imaging.
3) I had BCG as a child. Which test should I take?
An IGRA is often preferred because BCG can cause false-positive skin tests.
4) How soon after exposure should I test?
It can take 8–10 weeks after exposure for TST/IGRA to turn positive; if you test earlier and it’s negative, your provider may repeat it later.
5) What are common side effects of the TB Mantoux test?
Mild redness or itching at the site; a firm bump (induration) is what’s measured—not the redness. Serious reactions are rare.
6) What if my TB test is positive but my chest X-ray is normal?
You likely have latent TB infection. Your clinician may recommend preventive treatment (e.g., 3HP or 4R) to lower the risk of developing active TB.
7) How long do results take?
TST: Read at 48–72 hours. IGRA: typically 1–2 days. NAAT: hours to a day. Culture: weeks (needed for full drug susceptibility).
Source List (Authoritative)
- CDC: TST interpretation, process & BCG caveats; IGRA guidance; LTBI regimens; Xpert overview. CDC
- WHO/NCBI: Xpert MTB/RIF / Ultra policy & consolidated guidelines. World Health Organization
- ATS/CDC/IDSA: Diagnosis guidelines; management principles. IDSA
- NTCA: 3HP practical resources. tbcontrollers.org







Leave a Reply